At Empower Healthcare, we’re passionate about keeping our clients and our teams safe. Here’s everything you need to know about optimising manual handling in healthcare.
What is Manual Handling?
Manual handling encompasses any task where force is required to push, pull, lift, carry, lower, or restrain a person or object. In healthcare, this goes beyond simply assisting clients—it’s about ensuring their safety while protecting yourself.
Did you know manual handling injuries account for 58.9% of cases in healthcare, significantly higher than the 43.9% across all other industries (WorkSafe Victoria, 2007)?
Let’s explore how to stay safe while delivering quality care.
Understanding Your Spine
The spine is the structural backbone of the body, offering a stable foundation and safeguarding the nervous system. Its three natural curves—cervical, thoracic, and lumbar—play a pivotal role in maintaining proper posture and reducing strain.
Posture Tips:
• Keep your spine’s natural curves aligned for power and efficiency.
• Engage your deep abdominal muscles to stabilise the spine—think of it as a protective ‘corset.’ Hold that belly button in and breathe steadily!
Poor posture can lead to long-term damage, resulting in sprains, chronic pain, or worse.
Let’s minimise risks together.
Common Manual Handling Injuries
Healthcare workers are susceptible to a range of injuries, including:
• Muscle strains/sprains
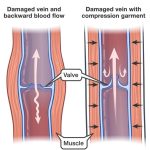
• Nerve compressions
• Joint damage (hands, shoulders, knees)
• Hernias and vascular issues
Identifying Hazards and Risks
Certain healthcare tasks—like lifting patients—cannot be fully avoided. This is where policies like the No Lift, No Injury Policy come in, aiming to:
• Minimise manual lifting of clients.
• Encourage the use of lifting aids like hoists and slides.
• Promote client independence wherever possible.
Manual Handling Best Practices
Here’s how to optimise safety during tasks:
Lifting
• Keep feet apart for stability.
• Bend knees, not your back.
• Keep loads close to your body.
Pushing
• Use your body weight for momentum.
• Maintain elbows close and a wide base of support.
Storage
• Store frequently used items at waist height.
• Avoid heavy items above or below shoulder level.
Teamwork
• Use clear communication (e.g., “Ready, set, go!”).
• Coordinate movements for efficiency.
Supporting Patient Transfers
Transfers are safer and smoother with attention to detail:
• Walking: Match your client’s pace and communicate clearly.
• Sit-to-Stand: Maintain good posture and provide balanced support.
• Slide Sheets: Use folding techniques and bed adjustments for bariatric clients.
Your Safe Handling Checklist
• Seek better, more efficient approaches to tasks.
• Avoid twisting—rotate the whole body from the hips.
• Ensure proper equipment is available and know how to use it.
• Call for help if you’re unsure or fatigued.
At Empower Healthcare, our commitment to safety is unwavering. Together, we can reduce risks and foster independence for all. Empower Healthcare is here to train and support your team, ensuring safety and independence for all.
If you have any specific questions or need further information, feel free to ask!
MORE BLOGS
The Rhythm of Recovery with Physiotherapy
…